Editor’s Note: This is the second story in a two-part series about proposed NIH funding cuts. The first story, published Monday, focused on the proposed policy changes and how research is funded at Notre Dame. Today’s story highlights the voices of scientists from laboratories across the University that may be impacted by the change.
Over 80 research projects at Notre Dame currently receive funding from the National Institutes of Health (NIH). The Trump administration’s proposed cuts to grants administered by the NIH could eliminate $7 million in federal funds from Notre Dame each year by capping facilities and administration costs at 15%, down from the University’s current rate of 56.5%.
If enacted, that change would significantly impact the way in which the University pays for research building maintenance and operation, shared lab equipment, hazardous waste disposal and utilities for NIH-funded projects.
The policy change, temporarily paused by order of a federal district court judge, has alarmed some scientists at the University. The Observer spoke to eight scientists to understand how their work might be impacted.
Felipe Santiago-Tirado
Felipe Santiago-Tirado, an assistant professor in the department of biological sciences, said his work has been funded by NIH since 2021. His team works on invasive fungal infections, specifically on Candida and Cryptoccocus neoformans.
“Not a lot of people know that fungi can kill you, but they can,” he said.
He described fungal diseases as a neglected type of infectious disease.
“We’re trying to figure out how do they cause disease, with the idea that if we now know how they cause disease, we can intervene and block it and then figure ways to either prevent it or treat those infections,” Santiago-Tirado said.
He has been awarded several grants from NIH, and currently has one active NIH grant, totaling $391,250. That includes $250,000 in direct costs and $141,250 in indirect costs.
He said that while the proposed funding changes have not had any practical effect on his work so far, he’s concerned about the ramifications if the change is enacted.
“I use core facilities in here to do my research, and those core facilities are supported by these indirect costs. What would happen to these core facilities? I don’t know if this doesn’t get resolved, you might imagine that the University will have to fire people that run these core facilities, and then at that point, I might get affected, because I need to use those core facilities,” he said.
Notre Dame currently has over 30 core-facilities, including the Notre Dame Integrated Imaging Facility, the Freimann Life Science Center, the Genomics and Bioinformatics Core Facility and the Zebrafish Core Facility.
Santiago-Tirado explained that core facilities are much more cost-effective because they are shared resources. Without core facilities, he explained, each laboratory would need their own equipment, which he said would less efficient. He used plasmid sequencing as an example.
“Everybody sequences plasmids in here. It makes no sense that everybody’s going to buy a sequencer. So [the] University has one, and it will make it available to everybody to use,” He said. “That is paid by, in part, by indirect costs.”
Santiago-Tirado pushed back strongly on the proposed 15% cap on indirect costs.
“I know some places might have very, very high indirects. And there might be ... ways to, like, cut that down. But just doing a flat 15% for everybody, irrespective of the type of institution, makes no sense,” he said.
He confirmed that he had received emails from University administration regarding the funding changes.
“They already told us, you know, document everything if you’re affected in any way, how you’re affected, but you should be able to keep submitting grants,” he explained.
However, he said news about NIH has been changing rapidly.
“I think the worst thing is this uncertainty,” he said.
Cristian Koepfli
Cristian Koepfli is also an assistant professor of biology at the University. His research focuses on the epidemiology of malaria.
“Malaria still is a major public health problem many countries of the world, roughly 600,000 people, mostly children, die each year from malaria, and about 200 million cases are observed,” Koepfli said.
He explained that while global health efforts made significant progress in the early part of this century, progress has largely stalled since 2015.
Koepfli’s NIH-funded project, which received $150,000 for direct costs and $84,750 for indirect costs, is focused on new interventions in Kenya to determine whether the interventions reduce the number of people with asymptomatic infections.
Koepfli said his team has collected and screened about 9,500 blood samples as part of the project.
“Then we look whether in those clusters or those villages where the intervention was introduced, we see a reduction in the number of people that carry the parasite,” he said.
He said that it is challenging not to know what the final decision on NIH funding will be and that cuts to the indirect rate would be felt throughout the University.
“The next time I should receive funding from the NIH will be in a couple of months, and I think until then we will see what happens,” he said.
Koepfli also added that malaria prevention efforts could be complicated by recent policy changes, including the dismantling of the United States Agency for International Development (USAID), an agency which has provided significant humanitarian aid in the past.
“I hope that … somehow, despite these big changes now, we will see [the United States] being a major player in the field of global health,” Koepfli said. “I mean children die that should not die because we have the drugs and the means to prevent them, and I believe, whatever your beliefs or your religion is, that is something good to do to help these populations.”
Olaf Wiest
Olaf Wiest, a chemistry and biochemistry professor, researches enzyme mechanisms. He has two NIH grants, one of which is focused on Ebola.
“This is about the biophysics of a certain protein involved in Ebola, which obviously is really bad for you, but it also is this very fascinating mechanism on how this enzyme, or this protein kind of changes over the cycle of the Ebola infection,” he explained.
He said that project has been funded for about six years.
The grant for Wiest’s other project, which focuses on an enzyme called HMG-CoA reductase, will expire at the end of July. Wiest said he is concerned about how he will be able to pay students if NIH grant review continues to be paused amid tumult within the medical research agency. He voiced frustration with what he described as the disruptive nature of the changes within NIH.
“I mean, we’re going to do research. But who's going to pay the students?” he asked.
Wiest said his lab has nine graduate students, two post-doctoral students and a staff member.
He also said that he believes the current indirect cost rate, or overhead rate, is “bare bones.”
“If you would do the same work in industry that overhead, again, physical facilities, administration, just the regulatory things to keep everybody safe, would easily be twice as much, quite probably more,” he said.
Matthew Webber
Matthew Webber is the acting director of the Berthiaume Institute for Precision Health at Notre Dame, which has over 70 faculty affiliates.
“Our faculty are among the most active in NIH submissions on campus,” he said, noting that the Boler-Parseghian Center for Rare Diseases and the Harper Cancer Research Institute also receive significant NIH funding.
He expressed the importance of waiting for a court ruling on the NIH funding decision.
“A lot of these issues are still to be adjudicated in courts and things like that, right? So it’s not like a lot of the issues are really touching faculties, budgets yet for research,” he said.
Still, he said that a cut from a 56.5% indirect cost rate to a 15% rate would be “major.”
“It’s going to be big, it’s going to be felt,” Webber said, while acknowledging that Notre Dame is less reliant on NIH funding than universities with larger medical research centers.
Webber voiced support for the current 56.5% indirect cost rate.
“I don’t think these [indirect cost] rates are outrageous. I think the way these rates are calculated is actually quite meticulous, and so I think there would be a decent amount of pain entailed in trying to restructure the way research is administered if cuts were down to 15%,” he said.
He also expressed worry that the 15% indirect cost rate could be expanded to other federal entities which fund research, including the National Science Foundation, the Department of Defense and the Department of Energy. Notre Dame received $27 million from the NIH last year, a fraction of the $134 million it received from all federal agencies combined.
“It’s up to the University to decide how to continue to support research efforts in the event that the federal government is no longer willing to fully support the cost of research,” he said.
In the meantime, Webber said that the University’s approach has been to continue operations as normal. He said the vice president of research Jeffrey Rhoads has advised researchers to continue submitting grants.
“I know some universities have paused or not allowed their investigators to submit NIH awards … I think Notre Dame is taking a different approach, which is basically, let’s keep doing business as usual until we see how things progress. I think that’s wise,” he said.
Webber said he’s neither optimistic nor pessimistic, but rather in a “wait and see” mindset.
“The initial phase of kind of political posturing and witch hunts and all of these other sorts of things kind of subside and we get to a stage where we can really focus on how to be a global leader in healthcare, research, in basic science and technology and these sorts of things,” he said.
Marya Lieberman
Marya Lieberman is a chemistry professor whose NIH-funded project is focused on developing a tool to detect poor-quality cancer medications in sub-Saharan Africa. She said the project has been funded almost entirely by NIH funds, receiving $448,376 in total project funds for 2024.
She said that while she thinks the proposed indirect rate cut has not affected her work yet, other disruptions have.
She said that a coordinating meeting between scientists at roughly two dozen research groups all working on low-cost techniques for improving cancer care was cancelled.
“We were planning a meeting to exchange information because there’s a lot of potential overlap between projects where a device that one group is developing might be useful for an implementation project that another group is doing. And so that coordinating meeting was just canceled,” she said.
Lieberman also brought up the logistical difficulties of grant administration that could be impacted if the indirect cost rate is cut.
“There’s a lot of really skilled people who do research administration, the keeping track of the budgets and ensuring that the money is being spent in the way that the contract designates … that’s kind of my main concern from a selfish perspective, because I’m not trained as an accountant.” Lieberman said. “So thinking about how to manage the the grants, they’re big, they’re complicated, and we want to do it right.”
Students at Notre Dame also benefit from NIH research grants, Lieberman said.
“I work with a number of undergraduate researchers ... and that kind of experience is really useful for students who want to go to graduate school to medical school. It’s really good training, and the student wouldn’t have had the opportunity without the NIH project,” she said.
Hsueh-Chia Chang
Hsueh-Chia Chang is a professor of chemical and biomolecular engineering who works on medical diagnostic devices. He said his research has been funded by the NIH for about a decade. In 2024, his project was funded with $150,000 for direct costs and $84,750 for indirect costs. In total, he said, NIH grants awarded to him and his collaborators have totaled roughly $5 million over the past 10 years, part of which supported PhD and postdoctoral students.
“My PhD and postdoc students have landed high-tech positions at Illumina, Sanofi, Merck, Alcon, Genentech, Mesoscale and many biotech startups. They have also accepted tenure-track faculty positions at NJIT, Rutgers, IU Indianapolis, Utah, Oregon State, UT San Antonio etc,” Chang wrote in a statement.
He said that four companies have licensed technologies his team invented as part of their NIH-funded work, including Aopia Biosciences, a California-based biotech startup.
“Aopia Biosciences … is currently commercializing a product ... based on a Notre Dame IP invented during one of my NIH projects. Aopia's Director of Engineering was a postdoc in my lab and was supported on an NIH grant,” Chang wrote.
The disruption to NIH’s grant process has impacted Chang’s work. He said that he is unable to hire or recruit new researchers with this uncertainty, and is reconsidering whether or not he will write future grant proposals. Additionally, he said that if NIH funding for his research is delayed or terminated, he will move up his retirement.
Richard Taylor
Richard Taylor is a professor of chemistry and biochemistry professor whose lab develops chemical and biological synthetic technologies and studies their potential as treatments for cancer and rare diseases.
He said that his lab has maintained continuous external funding support for over 25 years, which has included millions of dollars in funding from the NIH. His current project was funded with $380,849 for 2023.
He said that while his research program has not been directly affected yet, he is writing an NIH application with a March submission deadline that includes budget reconsideration.
Taylor expressed concern over sudden changes to NIH funding.
“A vast majority of the NIH funding, particularly here at Notre Dame, support research personnel and staff. Any disruption to this funding has serious consequences on these individuals that could discontinue their employment or delay their educational studies,” Taylor wrote in a statement.
While acknowledging the Trump administration’s desire to reduce federal spending, Taylor emphasized the importance of continued investment in health research.
“While even the biomedical researchers who are most affected would agree that there are ways to improve operational efficiencies, slashing funding for the infrastructure of country’s research and critical part of our scientific educational program is an error that will lead to damaging consequences to the engine that drives biomedical innovation in our country,” Taylor wrote.
Zachary Schafer
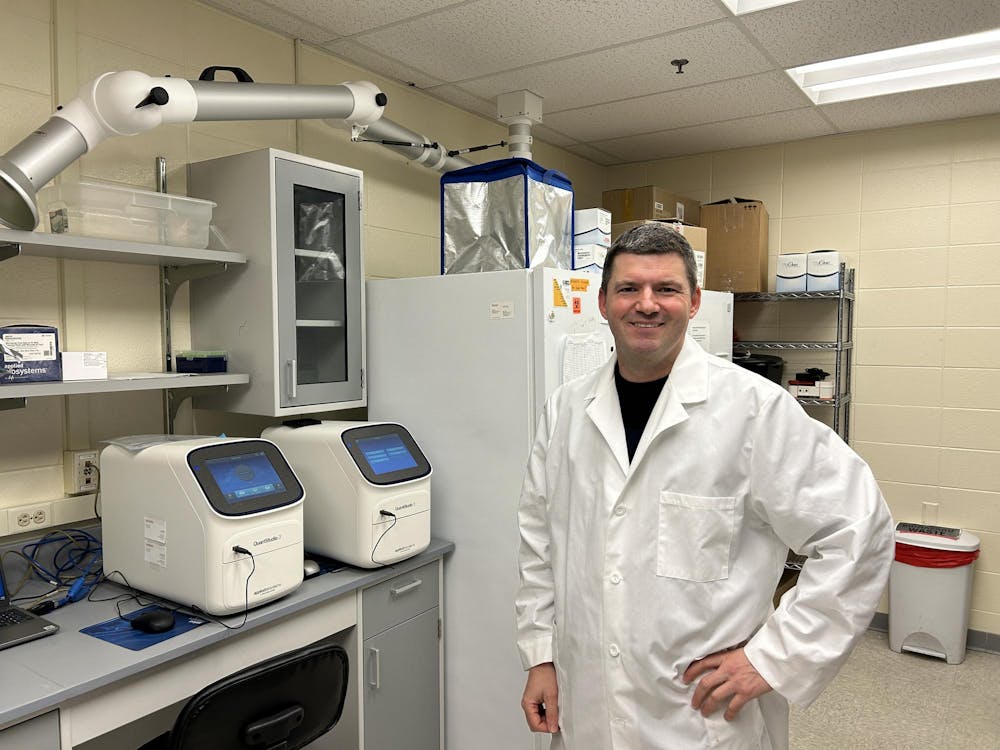
Zachary Schafer, a cancer biology professor, researches how cancer cells survive metastasis, the process by which cancer cells spread from a tumor to other parts of the body. In 2024, project received $241,966 for direct costs and $136,711 for indirect costs.
Funds for indirect costs pay for expenses including maintenance of laboratory spaces, biological waste disposal and compliance staff salaries, he said.
“These are real costs of doing high level research,” he wrote.
While his laboratory operations have yet to be disrupted, he said the proposed rate cuts would be devastating for labs at Notre Dame and throughout the country. In a written statement, he described the proposed 15% cap on indirect costs as “a huge overnight budget shortfall.”
“It means less dollars for cancer research, to study infectious diseases, to design better drugs, or to make new tools that enable new therapies,” he wrote.